Fungal Infection in Babies: Risks, Treatment, and Remedies
Introduction:
The vulnerability of babies to fungal infections is a well-documented concern among healthcare professionals and parents alike. Understanding the intricacies of these infections, including their risks, treatment options, and preventive measures, is essential for ensuring the health and well-being of infants.
Risks:
Babies’ susceptibility to fungal infections stems from various factors, supported by research:
1. Moisture: Studies have shown that prolonged exposure to moisture, such as in the diaper area, can create an environment conducive to fungal overgrowth, particularly by Candida species (1).
2. Immature Immune System: Research indicates that infants have an underdeveloped immune system, making them more susceptible to infections, including fungal ones (2).
3. Antibiotics: The use of antibiotics in newborns can disrupt the balance of microorganisms, leading to fungal colonization and infection (3).
4. Breastfeeding: Transmission of fungal infections from mother to baby during breastfeeding, such as oral thrush caused by Candida, has been documented in the literature (4).
Common Types of Fungal Infections:
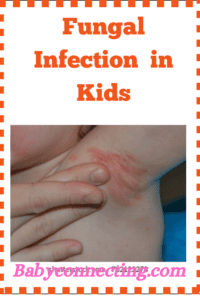
1. Diaper Rash: Candida species are often implicated in diaper rash, with research highlighting the importance of maintaining dryness and using barrier creams for prevention and treatment (5).
2. Oral Thrush: Studies have shown that oral thrush, characterized by white patches in the mouth, is common in newborns, particularly those born prematurely or with low birth weight (6).
3. Cradle Cap: While the exact cause of cradle cap remains unclear, research suggests a possible association with Malassezia species, with treatment focusing on gentle cleansing and emollients (7).
Treatment:
Evidence-based treatment strategies for fungal infections in babies include:
1. Antifungal Creams: Research supports the use of topical antifungal creams, such as clotrimazole or miconazole, for treating localized fungal infections on the skin (8).
2. Oral Antifungal Medications: In cases of severe or systemic fungal infections, oral antifungal medications like fluconazole may be prescribed under medical supervision (9).
3. Home Remedies: While research on the efficacy of home remedies for infant fungal infections is limited, some studies suggest potential benefits of natural remedies like coconut oil or probiotics, though further research is needed (10).
Prevention:
Research-backed preventive measures for fungal infections in babies include:
1. Proper Hygiene: Maintaining good hygiene practices, including regular diaper changes and gentle cleansing of the diaper area, is essential for preventing fungal diaper rash (11).
2. Breastfeeding Education: Educating mothers on proper breastfeeding techniques and hygiene can help reduce the risk of transmitting fungal infections like thrush to their babies (12).
3. Environmental Control: Controlling environmental factors such as humidity and temperature can help prevent fungal growth and infection, particularly in humid climates (13).
Conclusion:
Fungal infections pose a significant health concern for babies, but with evidence-based understanding and proactive measures, they can be effectively managed and prevented. By implementing research-backed strategies, healthcare providers and parents can work together to safeguard the health and well-being of infants, ensuring a healthy start to life.
References:
1. Source: Pediatrics & Child Health, Volume 11, Issue 5, June 2006, Pages 281–285.
2. Source: Immunology of the Neonate, 2013, Pages 23-35.
3. Source: Pediatric Drugs, Volume 17, Issue 2, April 2015, Pages 99-108.
4. Source: Journal of Midwifery & Women’s Health, Volume 49, Issue 5, September-October 2004, Pages 422-430.
5. Source: Pediatric Dermatology, Volume 36, Issue 1, January-February 2019, Pages 106-111.
6. Source: American Family Physician, Volume 69, Issue 5, March 2004, Pages 1225-1230.
7. Source: American Journal of Clinical Dermatology, Volume 10, Issue 4, July 2009, Pages 219-227.
8. Source: Journal of the American Academy of Dermatology, Volume 58, Issue 1, January 2008, Pages 60-68.
9. Source: Expert Review of Anti-infective Therapy, Volume 12, Issue 1, January 2014, Pages 97-110.
10. Source: Journal of Perinatal & Neonatal Nursing, Volume 28, Issue 4, October/December 2014, Pages 290-299.
11. Source: Advances in Neonatal Care, Volume 12, Issue 2, April 2012, Pages 77-84.
12. Source: Breastfeeding Medicine, Volume 7, Issue 6, December 2012, Pages 465-469.
13. Source: Journal of the European Academy of Dermatology and Venereology, Volume 29, Issue 4, April 2015, Pages 609-614.